Kingandu is a 2-day trip by car from Kinshasa (DRCongo). The first day is a rather comfortable drive of 520 km on a paved road to Kikwit, the city where the first Ebola outbreak started in 1995. A second full day is needed to cover the remaining 125 km on a dirt road to reach Kingandu. At least when everything runs smooth and it is dry season.
Once, Kingandu was a lively community of Jesuits. Now only a deserted church, almost the size of a cathedral, remains. Kingandu is also the location of a district hospital, providing healthcare support to 18 rural health centres and 121.000 people, covering an area of 2700 km2. Today, it is the centre of a pilot on telemedicine, where Dr. Alain and his team support nurses and midwives in the 3 surrounding health centres Sondji, Kimbimbi and Katenda, respectively 9, 6 and 28 km away, serving 20.000 people in 18 villages.

After spending a day in Kingandu, the project leader Dr. Jules, called by now ‘docteur lunette’ (doctor ‘smart glasses’) by the locals, takes us to Sondji, one of the rural health centres, to demonstrate how the telemedicine application works.
After several weeks of sensitizing the local community of Sondji, Dr. Jules started to educate Liliane, the main nurse, as well as some people of her team, consisting of 4 nurses and 1 midwife how to use Iristick smart glasses. Together they defined the operating procedures for a smooth tele-consult.
Every time a patient visits the rural health centre, Liliane makes a judgement: can she handle the case herself or does she need assistance from Dr. Alain and his team of 2 doctors in Kingandu.
In about 1 case out of 10, she decides to consult the doctors in Kingandu. Via the mobile phone, she sends a Whatsapp message and asks if one of doctors can be available in the next 10 to 15 minutes. In the meantime, she prepares the medical file of the patient. In the case of a pregnant woman, she wants to know for example the age and weight of the woman, whether it is her first baby, if there have been complications in the past, etc. Once ready, she puts on the smart glasses and calls the district hospital. She shares with the doctor, who sits behind his laptop, the medical record of the patient and then starts examining the patient with the help of the doctor. Thanks to the cameras in the smart glasses, the doctor has an ‘over the shoulder’ view of what Liliane observes and can freely communicate via speakers and mics. In the meantime, Liliane can fully concentrate on the patient, having both hands free to do any clinical examination necessary.
Upon arrival at the local health care centre, the people showed their gratitude for the project in a very warm way:
The real impact of smart glasses in Sondji
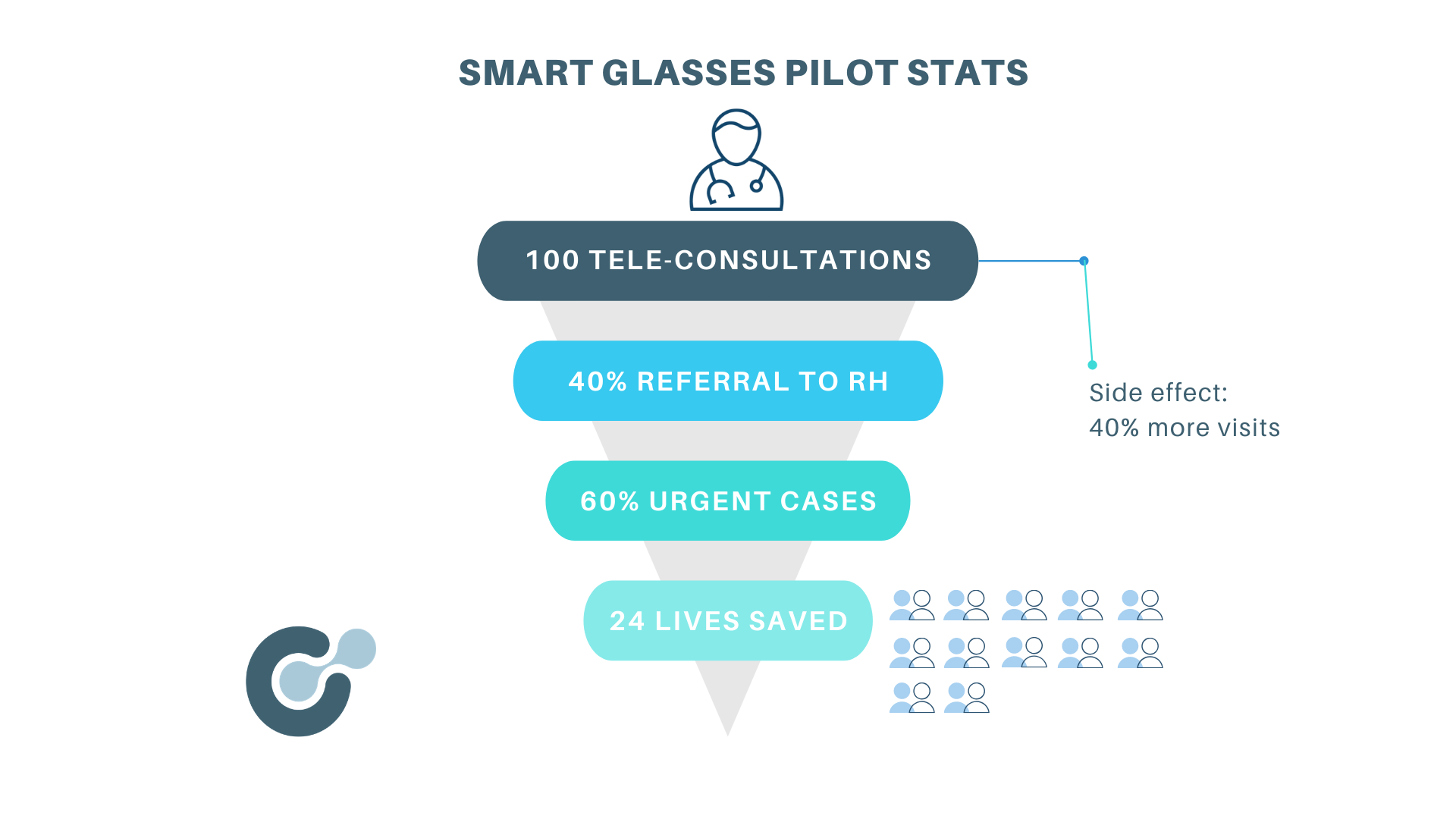
So far, about 100 tele-consultations have been executed over a period of 4 months, 50% related to maternal healthcare. These tele-consultations resulted over the past months in about 40% of the cases being referred to the district hospital for further treatment. 60% of the referrals was urgent. In such a case, a healthcare worker in Kingandu jumps on a motorbike (‘moto d’urgence’), re-built for medical transport, and drives to the rural health centre to pick up the patient within 3 hours.
Meanwhile the number of visits to the rural health centre has increased by 45% due to the trust and good reputation of the pilot. People feel they can get access to better quality healthcare and are taken seriously when urgency is needed. And more importantly, urgent cases do arrive in the district hospital, whereas previously, patients referred to Kingandu, often never arrived due to too long walking distance, family not willing to accompany the sick person or eager to look for a second opinion with the local medicine man.
The expectation is that, over time, once the 3 rural health centres are up and running in a couple of months, there will be about 15 to 20 tele-consultations per week, of which 5 will be urgent.
In parallel, we are introducing Rapid Diagnostics Tests in the rural health centres for diseases such as malaria, as well as some other tests, like pulse oximeters, and tests for hemoglobin and glycaemia. This will allow to dramatically increase the quality of local health care provision, as the nurses in the rural health centres will be trained and assisted by the lab people in Kingandu to use and interpret the test results via the smart glasses.
The future of this pilot
Although it is still too early for final conclusions, the pilot looks promising. Success would mean more people continue to visit the rural health centres because they trust the quality of the health care provided, while the percentage of referrals goes down because doctors in the district hospital provide better support to the local nurses via the smart glasses. Better diagnosis also means that only relevant cases are referred to the district hospital, where they will get the appropriate treatment and have a much better chance to survive.
A main challenge is the reliability of the online connectivity via VSATs as communication gets worse with heavy rains, tropical thunder and lightning. Intensive education and guidance of local healthcare workers remain crucial as well, not only in the application of the smart glasses, but also in the use of medical protocols and guidelines. The correct framing of the use of telemedicine is another constant point of attention. Some villagers are hoping to speak directly with Dr. Alain, seeing Liliane only as an intermediary person. This is of course the opposite of what we intend to achieve with this project, trying to re-enforce and strengthen the position of the frontline healthcare worker. Being both a technician and a medical doctor, Dr. Jules is very well positioned and working hard to overcome all of these challenges.
Finally, we would very much like to thank Memisa, who is doing an outstanding job in operationalising the idea of telemedicine thanks to their longstanding presence in rural DRC, their expertise in frontline healthcare and the trust they built over time with local communities. Prof. Wim Vandamme, professor Public Health at the Institute of Tropical Medicine in Antwerp, Belgium, who joined us during this visit, has been indispensable since the start of the project, providing very valuable advice and sharing his deep and broad experience. And without the team of Avanti, who installed the VSATs and provide the communication via satellites, this project would not have been possible. The commitment of their team to solve communication issues has been remarkable.

This project has been made possible thanks to the financial support of the Humanitarian Grand Challenge, a partnership of the U.S. Agency for International Development (USAID), the U.K. Department for International Development (DFID), the Ministry of Foreign Affairs of the Netherlands, with support from Grand Challenges Canada.
Steven Serneels, co-founder and chairman of Iristick